|
1.1 POJA-L653
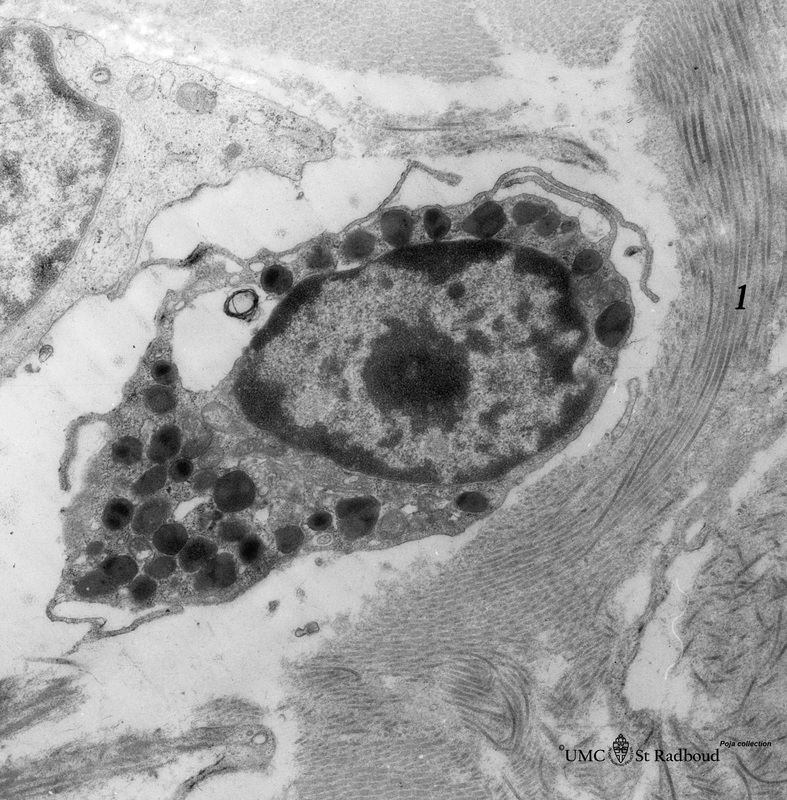
Title: Mast cell (lung, human) Description: Electron microscopy. Mast cells (mastocytes) are oval (12 mm) or spindle-shaped and show few thin microvilli at the surface. They are frequently found perivascularly or perineurally within the connective tissue (1). The cytoplasm is provided with a moderate amount of organelles. Most obvious is the presence of granules varying in shape and size. These membrane-bound vesicles (so-called compound granules) show a metachromatic reaction in light microscopy and ultrastructurally a granule exhibits a heterogeneous content (different with species) e.g. osmiophilic granular, filamentous, whorl-like substances. The granules contain among others heparin, histamine, enzymes such as superoxide dismutase, b-hexosaminidase, tryptase, factors such as neutrophil – and eosinophil-chemotactic factors, vasoactive mediators |
Background:
A second subset of mast cells is the connective tissue mast cell, the human connective tissue mast cells are also found in the skin and intestinal submucosa.
In humans, the corresponding subset is identified by the presence of several neutral proteases in the granules, including tryptase, chymase, cathepsin-G-like protease, and carboxypeptidase.
Mast cells are activated by cross-linking of the IgE-receptors occupied by IgE and by allergen. Activation of mast cells results in three types of response:
(1) secretion of preformed contents of their granules (exocytosis);
(2) synthesis and secretion of lipid mediators;
(3) synthesis and secretion of cytokines.
Analogous to basophilic granulocytes mast cells possess specific membrane receptors for the Fc segment of IgE produced in response to allergens. Eventually the release of the granular content by exocytosis (leading to degranulation of the mast cell) occurs resulting in e.g. an immediate hypersensitivity (anaphylactoid) reaction. The released biogenic amines (histamines) and the lipid mediators (PAF, PGD2, LTC4) cause vascular leak, bronchoconstriction and intestinal hypermotility. The newly synthesized cytokines (TNF) and said lipid mediators can induce inflammation. The enzymes released (tryptase) cause tissue damage.
Keywords/Mesh: blood, bone marrow, mast cell, basophilic granulocyte, metachromasia, histology, electron microscopy, POJA collection
A second subset of mast cells is the connective tissue mast cell, the human connective tissue mast cells are also found in the skin and intestinal submucosa.
In humans, the corresponding subset is identified by the presence of several neutral proteases in the granules, including tryptase, chymase, cathepsin-G-like protease, and carboxypeptidase.
Mast cells are activated by cross-linking of the IgE-receptors occupied by IgE and by allergen. Activation of mast cells results in three types of response:
(1) secretion of preformed contents of their granules (exocytosis);
(2) synthesis and secretion of lipid mediators;
(3) synthesis and secretion of cytokines.
Analogous to basophilic granulocytes mast cells possess specific membrane receptors for the Fc segment of IgE produced in response to allergens. Eventually the release of the granular content by exocytosis (leading to degranulation of the mast cell) occurs resulting in e.g. an immediate hypersensitivity (anaphylactoid) reaction. The released biogenic amines (histamines) and the lipid mediators (PAF, PGD2, LTC4) cause vascular leak, bronchoconstriction and intestinal hypermotility. The newly synthesized cytokines (TNF) and said lipid mediators can induce inflammation. The enzymes released (tryptase) cause tissue damage.
Keywords/Mesh: blood, bone marrow, mast cell, basophilic granulocyte, metachromasia, histology, electron microscopy, POJA collection