7.2 POJA-L1815+1817+1821
Title: Cervical intraepithelial neoplasm (CIN) (human, adult)
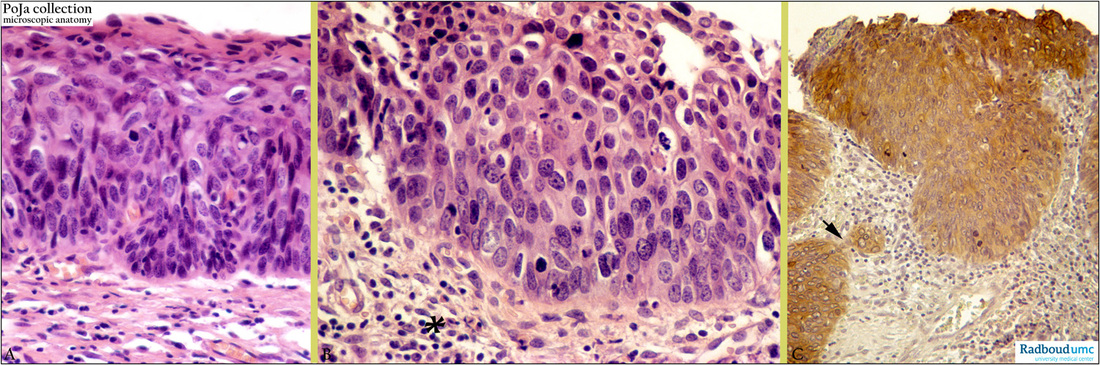
Description: Stain: (A-B) Hematoxylin-eosin; (C) antikeratin 7 antibody (OVTL 12-30) immunoperoxidase staining with diaminobenzidin reaction (DAB) and hematoxylin counterstaining.
(A): CIN 2 with mitoses and abnormal maturation in upper 1/3 of epithelium.
(B): CIN 3 with mitoses through full thickness of epithelium, loss of polarity, high N/C ratio, stroma with chronic inflammatory cells (*).
(C): CIN 3 with epithelium that distinctly expresses cytokeratin 7 with mitoses. From the lower border of the epithelium with CIN 3 features a CK 7-positive bud of suspect superficially micro-invasive squamous carcinoma (→) within a CK 7-negative stroma. (Partly by courtesy of G.P. Vooijs MD PhD, former Head of the Department of Pathology, Radboud university medical center, Nijmegen, The Netherlands).
Clinical background: The normal endocervical lining and cervical glands are usually positive for cytokeratin 7. At the squamocolumnar junction (usually in the ectocervix) multipotent reserve cells are nearby; they are cuboidal with round nuclei and scant cytoplasm becoming eosinophilic on maturing. They are involved in squamous differentiation especially in the transformation zone (= area between original squamocolumnar junction and border of metaplastic squamous epithelium). Proliferation of reserve cells expressing CK 7 leads to a multilayer. With increasing maturation it shows squamous differentiation resulting in squamous metaplasia and still preserve their CK 7- reactivity. Immunohistological studies of reserve cells indeed indicate presence of cytokeratin protein reserves of both columnar epithelial cells (low molecular weight keratin) as well as of non-keratinized squamous epithelial cells (high molecular weight keratin). Apparently reserve cells possess the potential towards a dual differentiation.
Keywords/Mesh: female reproductive organs., Cervix, CIN, keratin, cervical intraepithelial neoplasia (CIN), carcinoma in situ (CIS), uterine cervical neoplasms, histology, POJA collection.
Title: Cervical intraepithelial neoplasm (CIN) (human, adult)
Description: Stain: (A-B) Hematoxylin-eosin; (C) antikeratin 7 antibody (OVTL 12-30) immunoperoxidase staining with diaminobenzidin reaction (DAB) and hematoxylin counterstaining.
(A): CIN 2 with mitoses and abnormal maturation in upper 1/3 of epithelium.
(B): CIN 3 with mitoses through full thickness of epithelium, loss of polarity, high N/C ratio, stroma with chronic inflammatory cells (*).
(C): CIN 3 with epithelium that distinctly expresses cytokeratin 7 with mitoses. From the lower border of the epithelium with CIN 3 features a CK 7-positive bud of suspect superficially micro-invasive squamous carcinoma (→) within a CK 7-negative stroma. (Partly by courtesy of G.P. Vooijs MD PhD, former Head of the Department of Pathology, Radboud university medical center, Nijmegen, The Netherlands).
Clinical background: The normal endocervical lining and cervical glands are usually positive for cytokeratin 7. At the squamocolumnar junction (usually in the ectocervix) multipotent reserve cells are nearby; they are cuboidal with round nuclei and scant cytoplasm becoming eosinophilic on maturing. They are involved in squamous differentiation especially in the transformation zone (= area between original squamocolumnar junction and border of metaplastic squamous epithelium). Proliferation of reserve cells expressing CK 7 leads to a multilayer. With increasing maturation it shows squamous differentiation resulting in squamous metaplasia and still preserve their CK 7- reactivity. Immunohistological studies of reserve cells indeed indicate presence of cytokeratin protein reserves of both columnar epithelial cells (low molecular weight keratin) as well as of non-keratinized squamous epithelial cells (high molecular weight keratin). Apparently reserve cells possess the potential towards a dual differentiation.
Keywords/Mesh: female reproductive organs., Cervix, CIN, keratin, cervical intraepithelial neoplasia (CIN), carcinoma in situ (CIS), uterine cervical neoplasms, histology, POJA collection.