7.1 POJA-L1734+1507
Title: Epithelial inclusion cysts, ovary (human, adult)
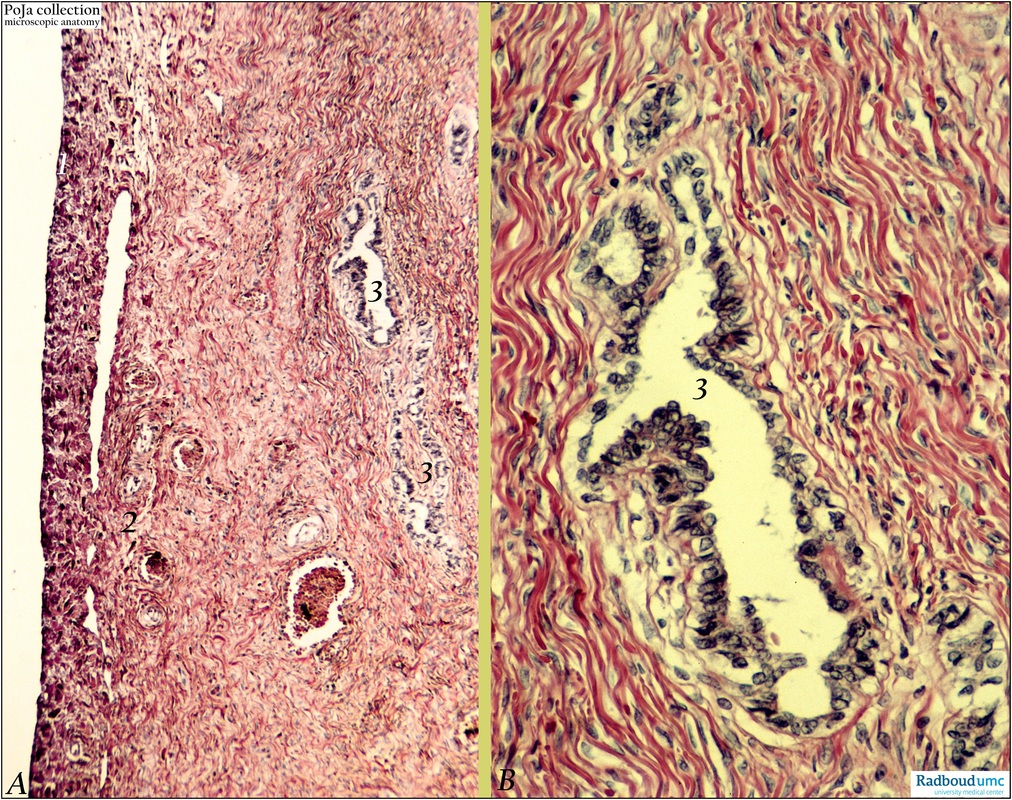
Description: Stain: (A, B) Hematoxylin-eosin.
(A): Surface of ovary (1), superficial cortex (2) with blood vessels and multiple inclusion cysts (3) of varying diameter.
(B): Enlargement of (A) show inclusion cyst lined by tuba-like epithelium.
Background: At any age single or multiple cysts are found in the superficial or deep cortex of the ovary varying in diameter from a few mm to several cm. These commonly hormonal inactive cysts derived from the surface epithelium are the so-called epithelial (or serous) inclusion cysts. They start as invaginations of the ovarian surface epithelium, then lose contact with the surface and develop into cysts due to accumulation of secretion. In most cases the epithelial lining resembles that of the fallopian tube, less frequently endometrioid or endocervical lining is found. Although ovarian serous tumors may arise from the ovarian surface epithelium or from epithelial inclusion cysts the pathogenetic mechanism is unknown and results are still contradictory. It is already suggested by Kurman (2010) that aggressive tumors e.g. high-grade serous carcinomas develop from the surface epithelium or inclusion cysts without morphologically recognizable intermediate stages (so-called “de novo” development). Low-grade serous carcinomas are associated with gene mutations (a.o ERBB2, KRAS) and develop stepwise-like from serous borderline tumors which may arise from the surface epithelium or from serous cystadenomas. It has been suggested by Kurman that serous ovarian carcinoma may well arise by implantation of tuba epithelium (Müllerian-type) into the ovary to form inclusion cysts and may further progress into ovarian carcinomas.
Keyword(s): female reproductive organs, ovary, inclusion cysts, female genitalia, ovarian neoplasms, serous cyst, histology, POJA collection
Title: Epithelial inclusion cysts, ovary (human, adult)
Description: Stain: (A, B) Hematoxylin-eosin.
(A): Surface of ovary (1), superficial cortex (2) with blood vessels and multiple inclusion cysts (3) of varying diameter.
(B): Enlargement of (A) show inclusion cyst lined by tuba-like epithelium.
Background: At any age single or multiple cysts are found in the superficial or deep cortex of the ovary varying in diameter from a few mm to several cm. These commonly hormonal inactive cysts derived from the surface epithelium are the so-called epithelial (or serous) inclusion cysts. They start as invaginations of the ovarian surface epithelium, then lose contact with the surface and develop into cysts due to accumulation of secretion. In most cases the epithelial lining resembles that of the fallopian tube, less frequently endometrioid or endocervical lining is found. Although ovarian serous tumors may arise from the ovarian surface epithelium or from epithelial inclusion cysts the pathogenetic mechanism is unknown and results are still contradictory. It is already suggested by Kurman (2010) that aggressive tumors e.g. high-grade serous carcinomas develop from the surface epithelium or inclusion cysts without morphologically recognizable intermediate stages (so-called “de novo” development). Low-grade serous carcinomas are associated with gene mutations (a.o ERBB2, KRAS) and develop stepwise-like from serous borderline tumors which may arise from the surface epithelium or from serous cystadenomas. It has been suggested by Kurman that serous ovarian carcinoma may well arise by implantation of tuba epithelium (Müllerian-type) into the ovary to form inclusion cysts and may further progress into ovarian carcinomas.
Keyword(s): female reproductive organs, ovary, inclusion cysts, female genitalia, ovarian neoplasms, serous cyst, histology, POJA collection