7.1 POJA-L1621+1561+1620
Title: Corpus luteum in ovary (human)
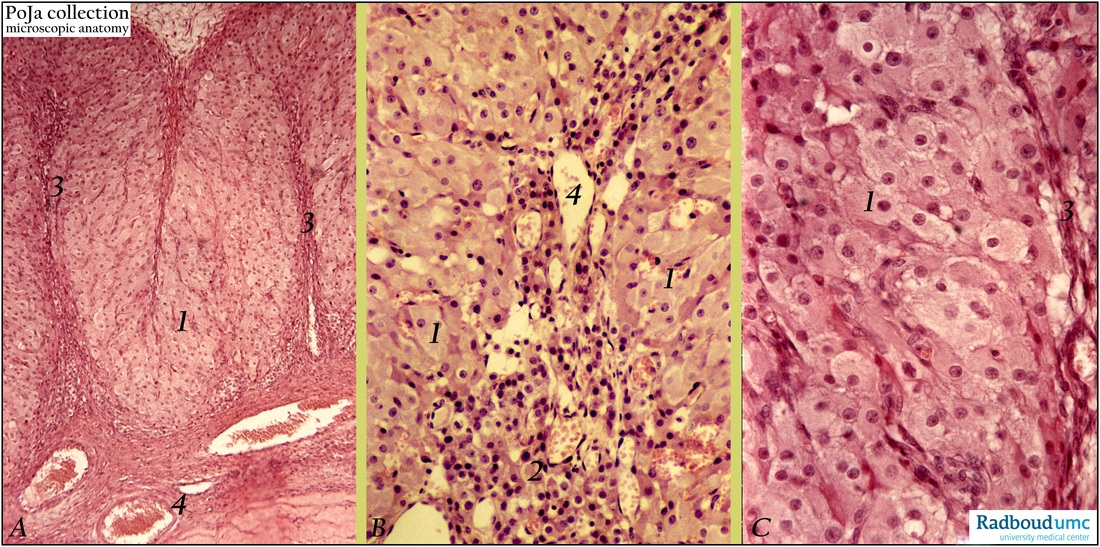
Description: (A, B, C) Stain: Hematoxylin-eosin;
(A): Low magnification of part of a corpus luteum of pregnancy (up to 25 mm) with epithelioid arranged sheets of round or polygonal lutein cells (1). Characteristically the corpus has a folded epithelioid wall with ingrown fibrous septa (3) richly supplied with blood vessels (4).
(B): Higher magnification shows the majority of larger granulosa lutein cells (1). Clusters of smaller theca lutein cells (or paralutein cells) (2) mostly localize peripheral close associated with septal connective tissue with thin-walled blood vessels (4)
(C): Mostly polygonal granulosa lutein cells (1) with foamy cytoplasm (lipids) and fibrous strand of septum at (3).
Background: After ovulation the lining stratum granulosum of the empty follicle collapses, becomes folded. Under influence of luteinizing hormone (LH) the luteinization, process starts i.e. the granulosa cells increase in size and differentiate into granulosa lutein cells while they produce a yellow carotenoid pigment (lutein) as well as progesterone/estrogen (in response to follicle-stimulating-hormone FSH and LH stimulation). Hence the name corpus luteum due to the yellowish color. The basal membrane of the collapsed follicle is broken down and internal theca cells invade in the cellular mass together with capillaries and connective tissue. The theca interna cells differentiate into theca lutein cells (or paralutein cells) and produce androstenedione and progesterone (in response to LH stimulation). The androgens from the theca cells are transformed into estradiol by the granulosa cells. Theca lutein cells together with the granulosa lutein cells form epithelial-like clusters or sheets (parenchyma) of round/ polygonal lutein cells storing fat droplets. The accompanying external theca cells provide stroma (3), septa of the enlarging corpus luteum that is supplied by numerous blood vessels (4) with supportive septa. Additionally many theca interna and externa cells involute and appear as small spindle-shaped cells. A corpus luteum of pregnancy (verum) persists until the fourth month with a diameter up to 25 mm (influence of human chorionic gonadotrophin, HCG) as a conspicuous yellow nodule in the ovary. Within and between the heavily luteinized granulosa cells eosinophilic hyaline globules are localized. Eventually the corpus involutes (luteolysis) with apoptosis, fatty degeneration of lutein cells, and autolysis. Removal by macrophages is followed by gradual replacement with fibrous tissue resulting in a large fibrous scar or corpus albicans. This scar decreases in size but will never disappear.
Keywords/Mesh: female reproductive organs, ovary, corpus luteum, granulosa cells, theca cells, pregnancy, paralutein cells, histology, POJA collection
Title: Corpus luteum in ovary (human)
Description: (A, B, C) Stain: Hematoxylin-eosin;
(A): Low magnification of part of a corpus luteum of pregnancy (up to 25 mm) with epithelioid arranged sheets of round or polygonal lutein cells (1). Characteristically the corpus has a folded epithelioid wall with ingrown fibrous septa (3) richly supplied with blood vessels (4).
(B): Higher magnification shows the majority of larger granulosa lutein cells (1). Clusters of smaller theca lutein cells (or paralutein cells) (2) mostly localize peripheral close associated with septal connective tissue with thin-walled blood vessels (4)
(C): Mostly polygonal granulosa lutein cells (1) with foamy cytoplasm (lipids) and fibrous strand of septum at (3).
Background: After ovulation the lining stratum granulosum of the empty follicle collapses, becomes folded. Under influence of luteinizing hormone (LH) the luteinization, process starts i.e. the granulosa cells increase in size and differentiate into granulosa lutein cells while they produce a yellow carotenoid pigment (lutein) as well as progesterone/estrogen (in response to follicle-stimulating-hormone FSH and LH stimulation). Hence the name corpus luteum due to the yellowish color. The basal membrane of the collapsed follicle is broken down and internal theca cells invade in the cellular mass together with capillaries and connective tissue. The theca interna cells differentiate into theca lutein cells (or paralutein cells) and produce androstenedione and progesterone (in response to LH stimulation). The androgens from the theca cells are transformed into estradiol by the granulosa cells. Theca lutein cells together with the granulosa lutein cells form epithelial-like clusters or sheets (parenchyma) of round/ polygonal lutein cells storing fat droplets. The accompanying external theca cells provide stroma (3), septa of the enlarging corpus luteum that is supplied by numerous blood vessels (4) with supportive septa. Additionally many theca interna and externa cells involute and appear as small spindle-shaped cells. A corpus luteum of pregnancy (verum) persists until the fourth month with a diameter up to 25 mm (influence of human chorionic gonadotrophin, HCG) as a conspicuous yellow nodule in the ovary. Within and between the heavily luteinized granulosa cells eosinophilic hyaline globules are localized. Eventually the corpus involutes (luteolysis) with apoptosis, fatty degeneration of lutein cells, and autolysis. Removal by macrophages is followed by gradual replacement with fibrous tissue resulting in a large fibrous scar or corpus albicans. This scar decreases in size but will never disappear.
Keywords/Mesh: female reproductive organs, ovary, corpus luteum, granulosa cells, theca cells, pregnancy, paralutein cells, histology, POJA collection